Overview

Heel pain is one of the most common conditions treated by podiatrists. It is often a message that something is in need of medical attention. Pain that occurs right after an injury or early in an illness may play a protective role, often warning us about the damage we have suffered. Heel pain is a problem which affects people of all ages and vocations, whether they are active or not and it comes in many different forms. Heel pain can also occur in children usually between the ages of 8 and 13, as they become increasingly active in sporting activities and during the growing phase.
Causes
In the majority of cases, heel pain has a mechanical cause. It may also be caused by arthritis, infection, an autoimmune problem trauma, a neurological problem, or some other systemic condition (condition that affects the whole body).
Symptoms
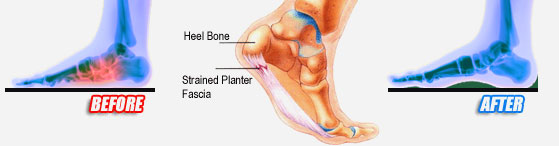
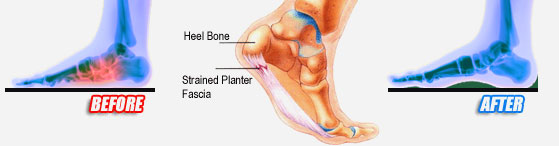
Depending on the specific form of heel pain, symptoms may vary. Pain stemming from plantar fasciitis or heel spurs is particularly acute following periods of rest, whether it is after getting out of bed in the morning, or getting up after a long period of sitting. In many cases, pain subsides during activity as injured tissue adjusts to damage, but can return again with prolonged activity or when excessive pressure is applied to the affected area. Extended periods of activity and/or strain of the foot can increase pain and inflammation in the foot. In addition to pain, heel conditions can also generate swelling, bruising, and redness. The foot may also be hot to the touch, experience tingling, or numbness depending on the condition.
Diagnosis
In most cases, your GP or a podiatrist (a specialist in foot problems and foot care) should be able to diagnose the cause of your heel pain by asking about your symptoms and medical history, examining your heel and foot.
Non Surgical Treatment
There are a number of treatments that can help relieve heel pain and speed up your recovery. These include resting your heel, try to avoid walking long distances and standing for long periods, regular stretching, stretching your calf muscles and plantar fascia, pain relief, using an icepack on the affected heel and taking painkillers, such as non-steroidal anti-inflammatory drugs (NSAIDs), wearing good-fitting shoes that support and cushion your foot, running shoes are particularly useful, using supportive devices such as orthoses (rigid supports that are put inside the shoe) or strapping. Around four out of five cases of heel pain resolve within a year. However, having heel pain for this length of time can often be frustrating and painful. In around one in 20 cases, the above treatments are not enough, and surgery may be recommended to release the plantar fascia.
Surgical Treatment
If treatment hasn't worked and you still have painful symptoms after a year, your GP may refer you to either an orthopaedic surgeon, a surgeon who specialises in surgery that involves bones, muscles and joints or a podiatric surgeon, a podiatrist who specialises in foot surgery. Surgery is sometimes recommended for professional athletes and other sportspeople whose heel pain is adversely affecting their career. Plantar release surgery is the most widely used type of surgery for heel pain. The surgeon will cut the fascia to release it from your heel bone and reduce the tension in your plantar fascia. This should reduce any inflammation and relieve your painful symptoms. Surgery can be performed either as open surgery, where the section of the plantar fascia is released by making a cut into your heel or endoscopic or minimal incision surgery - where a smaller incision is made and special instruments are inserted through the incision to gain access to the plantar fascia. Endoscopic or minimal incision surgery has a quicker recovery time, so you will be able to walk normally much sooner (almost immediately), compared with two to three weeks for open surgery. A disadvantage of endoscopic surgery is that it requires both a specially trained surgical team and specialised equipment, so you may have to wait longer for treatment than if you were to choose open surgery. Endoscopic surgery also carries a higher risk of damaging nearby nerves, which could result in symptoms such as numbness, tingling or some loss of movement in your foot. As with all surgery, plantar release carries the risk of causing complications such as infection, nerve damage and a worsening of your symptoms after surgery (although this is rare). You should discuss the advantages and disadvantages of both techniques with your surgical team.
heel pain exercises
Prevention
Heel pain is commonly caused from shoes that do not fit properly. In addition, shoes need to have ample cushioning and support, particularly through the heel, ball of the foot, and arch. Shoes should also be replaced if they become too worn. One sure sign of wear and tear is overly worn areas of a shoe's insoles. If the heel or ball of the foot is particularly worn, damage could easily occur since the bottom of the foot is not getting the cushioning it needs.

Heel pain is one of the most common conditions treated by podiatrists. It is often a message that something is in need of medical attention. Pain that occurs right after an injury or early in an illness may play a protective role, often warning us about the damage we have suffered. Heel pain is a problem which affects people of all ages and vocations, whether they are active or not and it comes in many different forms. Heel pain can also occur in children usually between the ages of 8 and 13, as they become increasingly active in sporting activities and during the growing phase.
Causes
In the majority of cases, heel pain has a mechanical cause. It may also be caused by arthritis, infection, an autoimmune problem trauma, a neurological problem, or some other systemic condition (condition that affects the whole body).
Symptoms
Depending on the specific form of heel pain, symptoms may vary. Pain stemming from plantar fasciitis or heel spurs is particularly acute following periods of rest, whether it is after getting out of bed in the morning, or getting up after a long period of sitting. In many cases, pain subsides during activity as injured tissue adjusts to damage, but can return again with prolonged activity or when excessive pressure is applied to the affected area. Extended periods of activity and/or strain of the foot can increase pain and inflammation in the foot. In addition to pain, heel conditions can also generate swelling, bruising, and redness. The foot may also be hot to the touch, experience tingling, or numbness depending on the condition.
Diagnosis
In most cases, your GP or a podiatrist (a specialist in foot problems and foot care) should be able to diagnose the cause of your heel pain by asking about your symptoms and medical history, examining your heel and foot.
Non Surgical Treatment
There are a number of treatments that can help relieve heel pain and speed up your recovery. These include resting your heel, try to avoid walking long distances and standing for long periods, regular stretching, stretching your calf muscles and plantar fascia, pain relief, using an icepack on the affected heel and taking painkillers, such as non-steroidal anti-inflammatory drugs (NSAIDs), wearing good-fitting shoes that support and cushion your foot, running shoes are particularly useful, using supportive devices such as orthoses (rigid supports that are put inside the shoe) or strapping. Around four out of five cases of heel pain resolve within a year. However, having heel pain for this length of time can often be frustrating and painful. In around one in 20 cases, the above treatments are not enough, and surgery may be recommended to release the plantar fascia.
Surgical Treatment
If treatment hasn't worked and you still have painful symptoms after a year, your GP may refer you to either an orthopaedic surgeon, a surgeon who specialises in surgery that involves bones, muscles and joints or a podiatric surgeon, a podiatrist who specialises in foot surgery. Surgery is sometimes recommended for professional athletes and other sportspeople whose heel pain is adversely affecting their career. Plantar release surgery is the most widely used type of surgery for heel pain. The surgeon will cut the fascia to release it from your heel bone and reduce the tension in your plantar fascia. This should reduce any inflammation and relieve your painful symptoms. Surgery can be performed either as open surgery, where the section of the plantar fascia is released by making a cut into your heel or endoscopic or minimal incision surgery - where a smaller incision is made and special instruments are inserted through the incision to gain access to the plantar fascia. Endoscopic or minimal incision surgery has a quicker recovery time, so you will be able to walk normally much sooner (almost immediately), compared with two to three weeks for open surgery. A disadvantage of endoscopic surgery is that it requires both a specially trained surgical team and specialised equipment, so you may have to wait longer for treatment than if you were to choose open surgery. Endoscopic surgery also carries a higher risk of damaging nearby nerves, which could result in symptoms such as numbness, tingling or some loss of movement in your foot. As with all surgery, plantar release carries the risk of causing complications such as infection, nerve damage and a worsening of your symptoms after surgery (although this is rare). You should discuss the advantages and disadvantages of both techniques with your surgical team.
heel pain exercises
Prevention
Heel pain is commonly caused from shoes that do not fit properly. In addition, shoes need to have ample cushioning and support, particularly through the heel, ball of the foot, and arch. Shoes should also be replaced if they become too worn. One sure sign of wear and tear is overly worn areas of a shoe's insoles. If the heel or ball of the foot is particularly worn, damage could easily occur since the bottom of the foot is not getting the cushioning it needs.




 The nerves located on the bottom of the foot between the metatarsal heads (the bone of the toe closest to the foot) supply feeling, or sensation, to the toes. One of these nerves may become irritated by the ligament located above it, causing it to become thickened and painful. Generally this problem occurs most often between the third and fourth toes, but it can occur between the second and third toes as well. It is uncommon for a neuroma to be located between the first and second or fourth and fifth metatarsals. Rarely is there more than one neuroma in a foot.
The nerves located on the bottom of the foot between the metatarsal heads (the bone of the toe closest to the foot) supply feeling, or sensation, to the toes. One of these nerves may become irritated by the ligament located above it, causing it to become thickened and painful. Generally this problem occurs most often between the third and fourth toes, but it can occur between the second and third toes as well. It is uncommon for a neuroma to be located between the first and second or fourth and fifth metatarsals. Rarely is there more than one neuroma in a foot.






 Overview
Overview Symptoms
Symptoms Symptoms
Symptoms RSS Feed
RSS Feed
